Feet and diabetes in the UK
In the UK, around 3.7 million people live with diabetes2
Diabetes prevalence in the UK is estimated to soar in the next few years and could reach 5 million by 20253. Diabetes bears a multitude of potential complications due to its vascular nature, foot complications being one of them.
If diabetes is not managed appropriately by the patient, the high blood glucose levels can cause severe issues and affect the patient quality of life. Diabetes can cause complications to the heart, the nerves (also known as neuropathy), the kidneys (nephropathy), the eyes and the feet.
Diabetes-related foot ulcers (also known as DFUs) are one of the most serious –and costly, complications of diabetes. They affect type 1 and type 2 patients alike.

Diabetes-related foot ulcers require a multitude of clinical skills for optimal management, and due to often poor healing outcomes cost the NHS nearly £1 billion per year4.
DFUs can take a very long time to heal. A study done in the UK found that at 12-month, only 35% of patients healed3, with amputation being an all too common outcome. All of the above make diabetes-related foot ulcers one of the most serious complications of diabetes. They pose a serious threat to patients’ lives, as well as a great challenge to clinicians.
Type 1 diabetes is an autoimmune disease, which results from destruction of the cells that make insulin in the pancreas. Insulin is vital because it regulates carbohydrate and fat metabolism. Loss of insulin secretion results in high blood glucose (also called hyperglycaemia). Insuline dosage should be monitored closely, as too much of it results in low blood sugar (or hypoglycaemia), which may lead to loss of consciousness.
Type 1 diabetes diabetes can occur at any age, but is most often diagnosed in children, adolescents, or young adults. It affects approximately 10% of all people living with diabetes in the UKx.
Type 2 diabetes is a chronic metabolic disease characterised by insulin resistance (that is, the body’s inability to effectively use insulin). The storage and release of energy from food is therefore not regulated, resulting in high blood glucose levels, which leads to chronic hyperglycaemia.
Type 2 diabetes affects 90% of people living with diabetesx, and usually occurs later in life, i.e. over the age of 40. It is commonly associated with obesity, physical inactivity and raised blood pressure.
- Foot ulcers are a complication for both diabetes types.
- Women can experience gestational diabetes during pregnancy but it usually disappears afterwards.
- Other rarer types of diabetes also exist.
What is a DIABETIC FOOT ULCER?
A diabetic foot ulcer is one of the most common, costly and severe complications of diabetes.
A diabetic foot ulcer is described by NICE as “an injury to the skin or underlying tissue (or both), below the ankle, in a person with diabetes” (NICE, 2015).
Several risk factors can lead a person with diabetes to develop foot ulcers, with Loss of Protective Sensation (caused by neuropathy) and Peripheral Arterial Disease (which leads to ischaemia) being the main factors.

MAJOR RISK FACTORS
Loss of Protective Sensation (LOPS) caused by neuropathy
Loss of Protective Sensation (later referred as LOPS) is caused by nerve damage, otherwise known as neuropathy. If a person with diabetes is affected by neuropathy, their ability to feel pain or other sensation (such as hot or cold) in their feet is compromised. This leads to trauma and injury to their feet to go unnoticed. Patients with LOPS may be unaware of pressure points on their feet from walking or footwear. This may lead to callus (harden skin) which is another risk factor for ulceration.
A patient can suffer from LOPS (caused by neuropathy) and ischaemia (caused by Peripheral Arterial Disease).
Patients with LOPS could step on glass, or on a very hot surface such as sand without noticing it.

Foot deformities
Foot deformities are a frequent occurrence when a person with diabetes suffers from neuropathy, due to a weakening of the muscles and a change to the shape of the foot. They pose a challenge and a threat especially since patients with neuropathy do not feel pressure or friction caused by those deformities, which can lead to ulceration.
Peripheral arterial disease (PAD) which leads to ischaemia
Peripheral Arterial Disease is associated with diabetes, and causes a poor blood supply to the legs. It is caused by the narrowing of arteries, which limits the blood flow and thus the delivery of oxygen and micronutrients to the legs and feet. It compromises the natural wound healing trajectory, amongst other things.
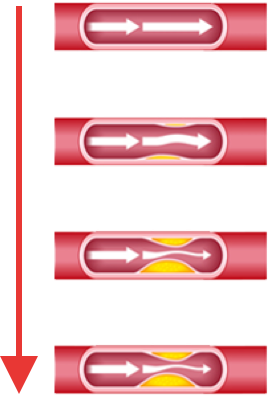
When a limb does not get a good enough blood supply due to narrowed or blocked artery, it can become ischaemic (the patient would have ischaemia). Once the PAD becomes very severe, the patient can experience critical limb ischaemia (when oxygenation of the limb tissue is compromised) or gangrene. Any one of those factors should be ground for immediate patient referral to the closest specialised care setting.
A patient can suffer from ischaemia (caused by Peripheral Arterial Disease) and LOPS (caused by neuropathy) simultaneously.

Patient own history of foot ulceration or amputation
In the UK, previous foot ulceration or amputation put the patient in the high risk category5, which stresses how critical of a risk factor they are. Why is that? Because once a patient developed his or her first diabetes-related foot ulcer, they are highly likely to develop another in the future.
40% of patients with previous foot ulcerations will develop a new foot ulcer within 1 year. The number goes up to 65% after 3 yearsx. Furthermore, amputation is also a major risk factor, and is associated with very poor patient outcomes: 70% of patients who have one won’t be alive within 5 yearsx. In the UK, 10% of patients with a diabetic foot ulcer will end up with an amputation.
/!\ Diabetic foot ulcers are very prone to infection, which can lead to amputation. A diabetic foot ulcer lasting more than 30 days becomes 4 times more likely to get infected(xx).
THE 3 AETIOLOGIES OF DIABETIC FOOT ULCERS
Every DFU aetiology will require a different approach when building the care plan, which is why correct identification is crucial.
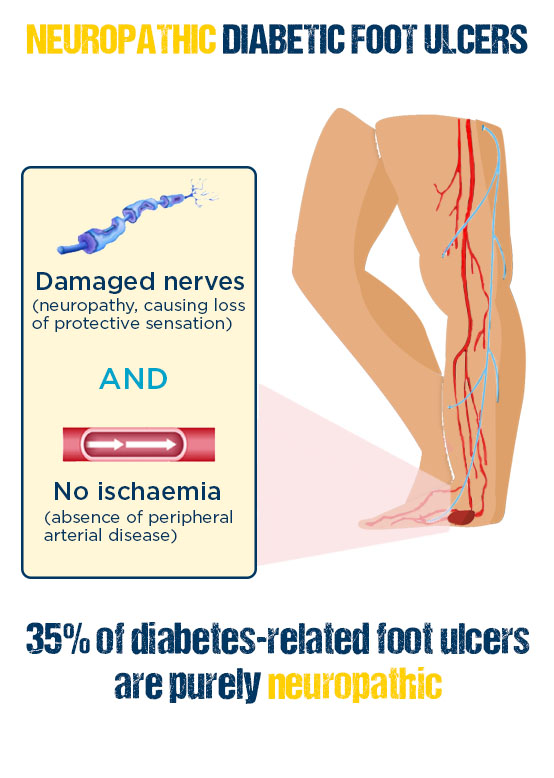
Neuropathic diabetic foot ulcer
Neuro-ischaemic diabetic foot ulcer

Ischaemic diabetic foot ulcer

Neuropathic foot ulcer
- Etiology: damaged nerves
- Wound bed: pink and granulating
- Location: weight bearing areas (metatarsal heads, heel, over the dorsum – claw toes)
- Sensory loss
- Callus present and often thick
- Dry skin and fissuring (cracks)
- Hyperkeratosis
- Foot deformities
- Foot warm with bounding pulses
Ischaemic foot ulcer
- Etiology: restriction of arterial blood flow
- Painful
- Necrosis common
- Foot cold without pulses
- Wound bed: pale and sloughy with poor granulation tissue
- Location: tips of toes, nail edges, between the toes and lateral borders of the foot
Neuro-Ischaemic foot ulcer
- Etiology: both nerves function and arterial supply
- Degree of sensory loss
- Variable callus
- Prone to necrosis
- Foot cold without pulses (potentially)
- Wound bed: poor granulation tissue
- High risk of infection
- Location: margins of the foot and toes, everywhere on the foot
consequences of diabetic foot ulcers

every 20
seconds4
 every 20
every 20 seconds4
70% of patients 5
 70% of patients 5
70% of patients 5
85% of amputations1
 85% of amputations1
85% of amputations1
DIABETIC FOOT ULCERS ARE A HUGE BURDEN
The quality of life for patients with active diabetes-related foot ulcers is very poor. Isolation is very common, with many patients unable to go to work or pursue normal activities and social interactions(xx).
Patients’ quality of life is made even worse by the long healing time of those wounds: in the UK, a study found that at 12 months, only 1 out of 3 patients were healed. Almost half of diabetic foot ulcers remained unhealed, and for many the outcome was amputation(3).
Diabetes causes 169 amputations a week in England(6). The worldwide figure is even more shocking: diabetes causes an amputation every 20 seconds(7), making it the world leading cause of amputation.
The bad news is, be it in the United Kingdom or in the world, the number of amputation is on the rise. The good news is, up to 85% of amputations could be prevented.
IN THEIR OWN WORDS
Discover real testimonials of patients who experienced diabetes-related foot ulcers.
1. Setacci C, de Donato G, Setacci F, Chisci E. Diabetic patients: epidemiology and global impact. J Cardiovasc Surg (Torino). 2009 Jul, 50(3) : 263-73
2. International Diabetes Federation Atlas – 9th edition 2019
3. Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017 Jun 15;376(24):2367-2375.
4. Whiting, D. R., Guariguata, L., Weil, C., and Shaw, J. 2011. “IDF Diabetes Atlas: Global Estimates of the Prevalence of Diabetes for 2011 and 2030.” Diabetes Res. Clin. Pract. 94 (3): 311-21.
5. Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med 2017; 376: 2367–75.
6. Moxey PW, Gogalniceanu P, Hinchliffe RJ, Loftus IM, Jones KJ, Thompson MM, et al. Lower extremity amputations–a review of global variability in incidence. Diabet Med. 2011 Oct;28(10):1144–53; DOI:10.1111/j.1464-5491.2011.03279.x.
Every healthcare professional has a key role to play to save feet, and save lives.


